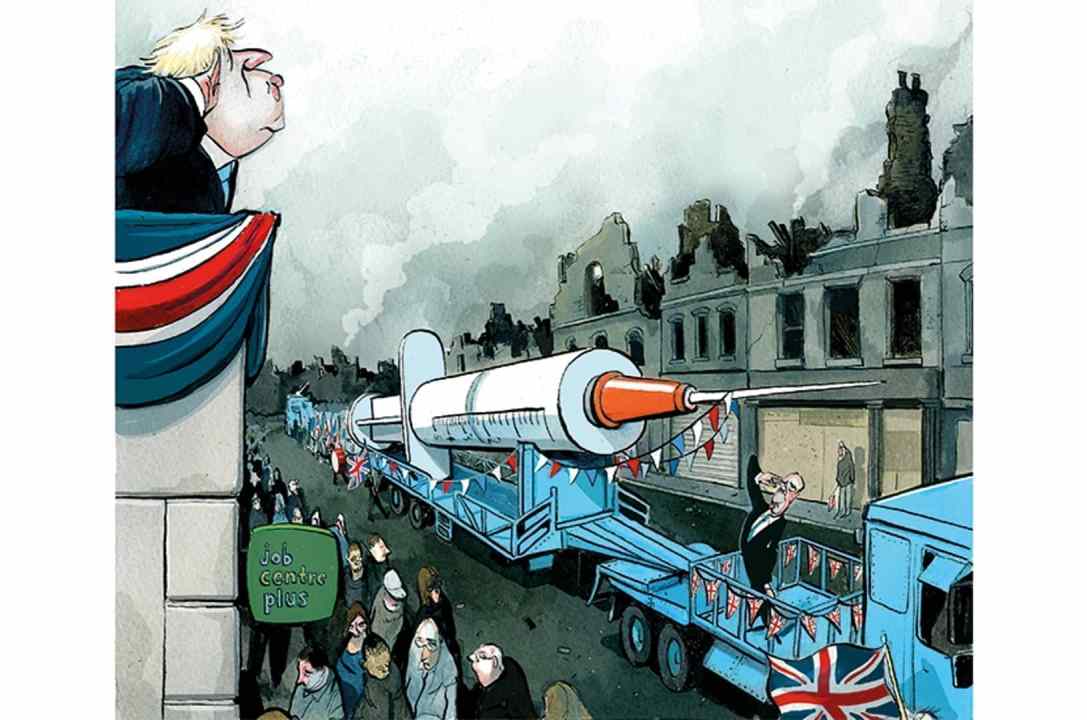
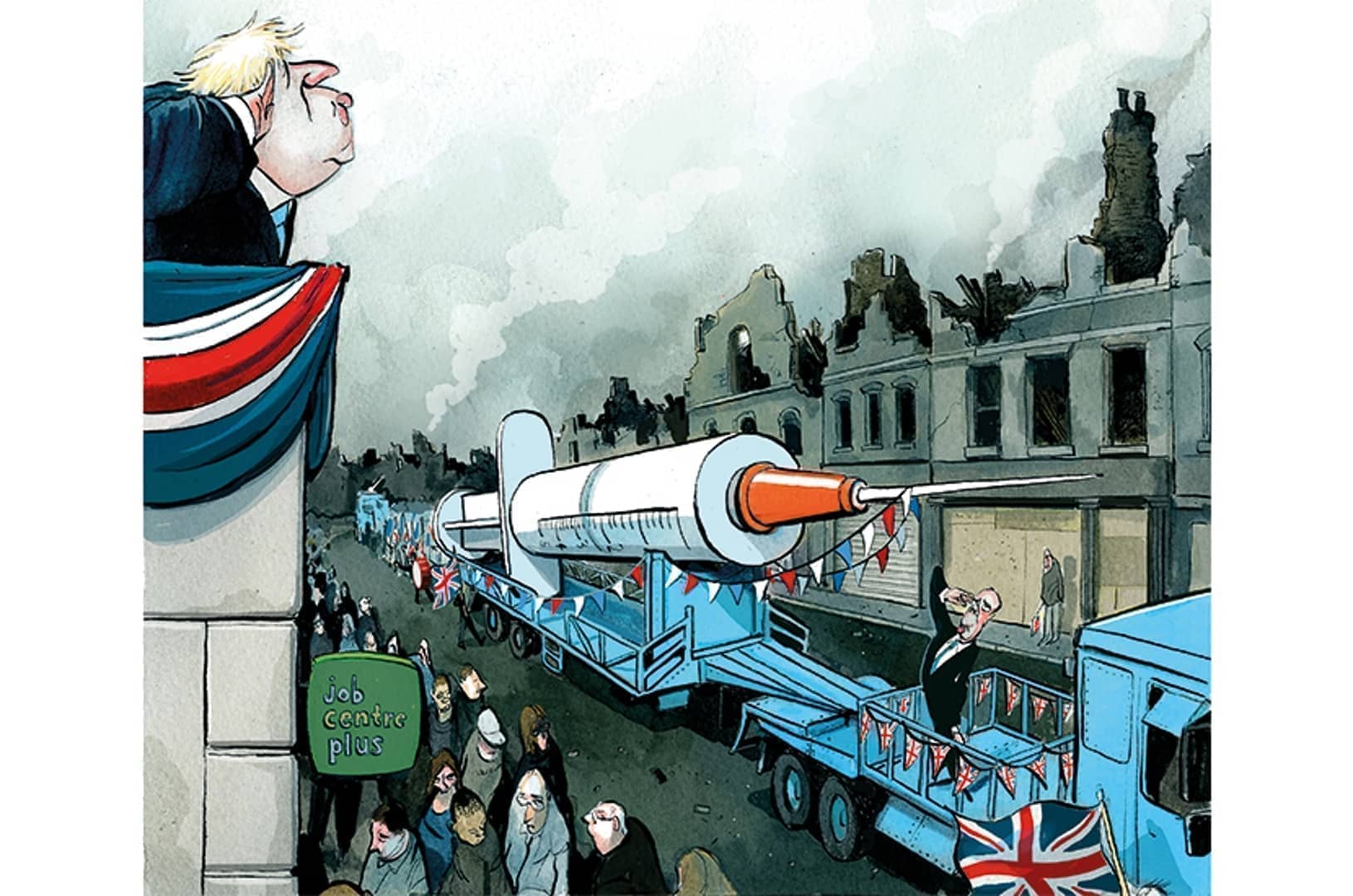
How should we treat the unvaccinated? Should we stop them from participating in normal life? Castigate them in the media? Mandate they get vaccinated or block them from accessing NHS services?
It’s a creeping question across developed countries — asked on Good Morning Britain’s Twitter page yesterday, and then subsequently deleted. Germany has barred the unvaccinated from most aspects of public life, including shops and restaurants. Greece is charging the over-60s Є100 for every month they remain unvaccinated, with money going to top up the health services. In Singapore, the unvaccinated will no longer have their Covid care paid for by the state. A letter in the Times this week suggested the same should happen here too.

In the UK, resentment towards the unvaccinated is growing, as some try to draw a direct link between their un-jabbed status and looming restrictions. In response to the news that, between July and November, 90 per cent of patients receiving specialist care had not received the Covid jab, frontline staff have expressed frustration at the number of unvaccinated patients passing through the health service, with the chairwoman of the British Association of Critical Care Nurses declaring:
All nurses understand they have to provide non-judgmental care. But what we find difficult is that giving care to patients who have chosen not to be vaccinated has a knock-on effect on other patients. We are still human beings and we still get angry at things that we think aren’t just.
Publicly shaming the unvaccinated is anathema to the values of personal autonomy or individual responsibility
Meanwhile, one anonymous respiratory consultant informed the Guardian last month that in hospital Covid has largely become a disease of the unvaccinated, leaving their patience ‘wearing thin’. The British Medical Association is suggesting that it’s the unvaccinated that are ‘seriously limiting’ the NHS’s ability to treat other patients, stoking division between the jabbed and the un-jabbed.
How long, therefore, until the clamour for barring the unvaccinated from public services and public life — or introducing our own pass sanitaire — starts to mount here? Exasperation at the unvaccinated is to be expected — and is presumably directed at anti-vaxxers rather than the small minority unable to receive the jab for medical reasons. But the more ‘overwhelmed’ our state-run healthcare system, the more taxpayers will be pitted against one another according to the lifestyle choices they make.
Those currently lambasting the unvaccinated for clogging up the NHS should be careful what they wish for. If we demonise one group on one populist ground, it won’t be long before the fanatics open another front. Should we denounce over-eaters, drug addicts, even those who drive, walk or cycle to work? Based on hospital admissions data, these are all activities or choices that could consume precious NHS resources. Should we also ask jockeys to hang up their riding boots or mountaineers to put down the carabiners?
Restricting liberties to avoid pressure on the NHS is only half of the problem with the anger against the unvaccinated. The other issue is that not all the jab hesitant are anti-vaxx conspiracy theorists who believe a group of elites are using Covid-19 as a means of social control, and too little effort has gone towards understanding the reasons behind any suspicion towards the vaccine.
As The Spectator data hub shows below, there is significant demographic variation in vaccine uptake. 31 per cent of unvaccinated over-50s are black. 15 per cent are South Asian, and 6 per cent white. Data from July showed that 21.3 per cent of White British healthcare workers (HCWs) are vaccine hesitant, compared to 54.2 per cent of Black Caribbean or 33 per cent Chinese HCWs. This isn’t a Covid phenomenon: there is clear evidence that children from some ethnic groups are much less likely to be immunised than others.
Tailoring communications towards those groups less likely to receive the jab is vastly more likely to increase uptake than lambasting them across the media or suggesting they should be excluded from parts of our society. The same could be said of improving access to primary care, or targeting hard-to-reach groups through education, advertising and community initiatives.
The case for adopting more effective strategies to increase uptake extends beyond the potential benefits to our healthcare service. 23.4 per cent of ‘Asian,’ 28.6 per cent of ‘Pakistani/Bangladeshi’ and 15.2 per cent of ‘Black’ employees work in ‘distribution, hotels and restaurants‘ — sectors where labour shortages are most acute. If those workers are self-isolating, or even hospitalised with Covid, business will suffer. And the more needles in arms, the less likely a renewed lockdown which could come at a cost of £6 billion per month.
Publicly shaming the unvaccinated is anathema to the values of personal autonomy or individual responsibility. Both are immoral and, with hospital occupancy remaining low, unnecessary. If we insist on living in a nation with centralised healthcare, we cannot also live in one where protecting an institution, however beloved, limits the choices we make.
This article is free to read
To unlock more articles, subscribe to get 3 months of unlimited access for just $5





Comments
Join the debate for just $5 for 3 months
Be part of the conversation with other Spectator readers by getting your first three months for $5.
UNLOCK ACCESS Just $5 for 3 monthsAlready a subscriber? Log in