It was never the plan for the NHS to deal with a second wave of Covid. The official strategy, all through the summer, was for the £12 billion Test and Trace system to come along and zap new cases. Decisions for NHS investment this winter were made on the assumption that hospitals would be fine – because Dido Harding’s new system would work – this is why the Treasury rejected funding for the rollout of NHS ‘Seacole Centres’ for Covid convalescents. But the expensive system failed and the NHS is back in the hot seat. Whether this is a second wave or (as the WHO has argued) smaller ripples after the end of the first wave, the question is how much of a risk it poses. No.10 is trying to persuade Manchester to accept Tier 3 restrictions by claiming that ‘hospital admissions in Greater Manchester are doubling every nine days’ and that the hospitals are at capacity. But what’s the evidence for this – and other claims of NHS overflow?
Matt Hancock, the Health Secretary, has gone back to Plan A, reviving his ‘protect the NHS’ message from March and now wears a facemask with those words on it. The Prime Minister is repeating the slogan. It’s deeply controversial with senior doctors who fear that it discourages the sick from seeking help – which might explain the 28,000 excess at-home deaths over the last few months. The NHS is worried about this and has countered with its own advert, urging people to seek medical help. I looked at this in my latest Daily Telegraph column.
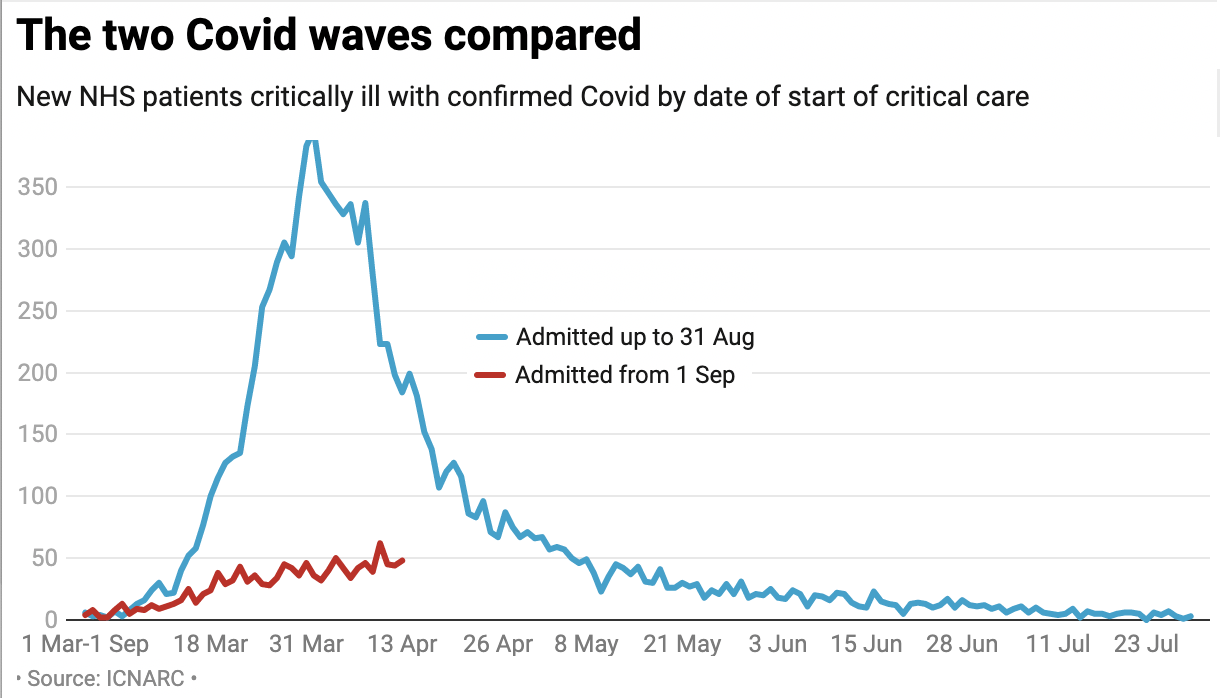
The NHS has learned much from the first wave of Covid. PPE equipment, for example, is now in bountiful supply. Basic medical techniques – better use of blood thinners, oxygen therapy, steroids etc – are having a big impact on survival rates. When Boris Johnson went into intensive care, his survival chances were about 50 per cent. Now, they would be closer to 70 per cent. The trajectory this time is nowhere near as daunting – the below graph shows the rise of Covid patients needing critical care. As the data shows, intensive care unit (ICU) usage is 13 per cent of what it was at the end of March. (These figures are from the Intensive Care National Audit & Research Centre.)
This time, as with last time, the number of Covid-related deaths tracks ICU usage. It shows a second wave very different to the first: so far, at least.
Merseyside has been at the eye of the new Covid storm: medically and politically. The narrative of NHS overcapacity is being deployed by local and national authorities to promote adherence to lockdown measures, but the statistics used in this debate are strikingly selective. Liverpool University Hospitals had 320 Covid patients earlier this week, vs 400 at the peak last time. But zoom out and the situation is very different: there are about 350 Covid patients in hospitals across the whole of South West and South East England, for example. So the Liverpool situation is not a proxy for the NHS more widely.
Should Liverpool’s 90 ICU beds become full, plans are in place for an extra 30 ICU beds: this is the “surge capacity” in every hospital, another reason why the stats are misleading. If things get busy, capacity will be added, routine surgery delayer or patients routed to other hospitals. This is how the NHS works. It’s a world leader in scaling up – and triage. There are other hospitals within half an hour’s drive (in St Helens and Clatterbridge, for example) that can take patients. There are many ways of creating capacity in hospitals, and that’s before you get to the Nightingale overflow units. Elective operations can be delayed – which of course creates problems down the line. But there are many ways to stop hospitals being overwhelmed: as the NHS demonstrated so strikingly – I’d say heroically – during the first wave.
In the politicised debate over the NHS in Liverpool, we often hear that its ICUs are running at 90 per cent of capacity. But this is pretty normal for an NHS hospital: over the past ten years, ICU occupancy in Liverpool has always been between 80 per cent and 90 per cent. Nationally, ICU usage is at 60 per cent – far below normal. Nationally, there are about 475 Covid patients on ventilators across the NHS, with 4,750 ventilator beds available. So it’s hard to use these figures to point to a health service at risk of collapse, or anywhere close to collapse. The NHS in Liverpool is coping strikingly well,
The issue is more the staff, and the 14-day quarantine rules that kick in if, for example, your kid is off school. About 12 per cent of nurses in Liverpool University Hospitals are currently off work. Updating quarantine rules for nurses (i.e., allowing them to work if they test negative to Covid) is one way of reducing this risk.
It’s also worth looking at London, which is now under the Tier 2 restrictions that Sadiq Khan has long been lobbying for. The capital was hit hard first time around, with hospitalisations peaking at 880 a day. Now, they are not doing even a tenth of that. We have not been told much about why London is being put into Tier 2 – but it certainly isn’t to ‘protect the NHS’.
Of course, the concern is the lag: where the NHS will be in a fortnight’s time, which can be gauged, more or less, from today’s infection rates. In Manchester, the concern is that it’s two to three weeks behind Liverpool in the infection curve (although case growth in the city has been calmer recently). But even if the hospital load trebles, the NHS could cope. You can look beyond a fortnight, and come up with bigger Covid forecasts – but the error margin in the projections becomes unworkable. As we have seen.
In mid-March, for example, the advice coming out of Sage was that there could be 90,000 Covid patients needing intensive care – quite a challenge for an NHS with only 100,000 beds in total. Britain was badly hit, but the peak demand for ventilators was 2,881. This shows the problem of four- to five-week extrapolations. If cases had doubled every seven days, as per that now-famous Vallance graph, there would be a major NHS problem. But the actual trajectory has proven rather different.
It’s the job of Sage to come up with ‘reasonable worst case’ scenarios in pandemics. But if the NHS worked on that basis, it would be cancelling thousands of non-Covid operations in preparation for something that is unlikely to arise –thereby risking far more lives than would be saved. The SPI-M projections, provided to Sage, should be taken with a pinch of salt: that’s obvious not just from the Vallance graph above, but from the figures churned out by Sage mid-March that were out by a factor of 30. I do wonder if No.10 is making policy now based on the SPI-M worse-case scenarios, with the attendant error margins. A policy of agile response and a two-week planning horizon – as the NHS is now operating on – makes more sense.
The Vallance graph was an illustrative scenario, not a prediction. But it is still useful, serving as a reminder of how simple projections of Covid can be deeply misleading (like the Imperial College forecasts for Sweden) and risk needless damage to the economy, society and public health.
This brings us to No.10’s attempt to persuade Manchester to accept its Tier 3 measures. it deployed the Vallance technique: claiming that ‘hospital admissions in Greater Manchester are doubling every nine days’. The use of the present tense – ‘doubling’ – is not supported by the data. If a figure doubles, why assume it will keep on doubling? The key error is the assumption of linearity in Covid growth. The rate of growth in cases has, in fact, been slowing steadily for some time.
Hospital admissions lag new cases by 10 to 14 days – but new cases actually peaked in Manchester earlier this month and are now falling. The below shows Covid test data by specimen data (as opposed to reporting date).
That Covid cases peaked weeks ago in Manchester is never acknowledged by No.10. But candour matters. If people in Manchester are wrongly told that the hospitals are ‘overrun’ then people who need NHS help (if they feel chest pain, for example) are less likely to seek it. This is the danger posed by exaggerated reports. One recent headline claimed ‘Covid: Greater Manchester running out of hospital beds.’ This is flatly untrue and was later changed online to ‘critical care beds’ – but how much evidence is there for even this?
By Friday 211 of the 257 critical care beds in Greater Manchester – 82 per cent of the total supply – were already being used for either those with Covid or people who were critically ill because of another illness.
What the report does not say is that 82 per cent occupancy is standard for Manchester critical care beds. ICU units are very expensive to run, hospitals ration their use carefully. We looked up the data since the start of 2018 to put the latest figure – 82 per cent occupancy – in context.
I have several criticisms of the NHS – why, for example, can’t it publish daily, easy-to-read regional ICU data like France does to reassure people worried about overload? It might be argued that exaggerating NHS capacity is a noble lie: that it may be unduly alarmist, but would prompt people to change behaviour and slow the threat of Covid. But against this we have to set the recent rise in home deaths from heart attacks and other conditions that would be treated in A&E if people had not been wrongly told that hospitals are at or near capacity. This isn’t about spin. Honesty is needed when discussing public health because the lack of it can cost lives.
When figures are vague and data hard to find, it gives scope for huge misunderstandings – which politicians can exploit. It would be shame if this were to happen now, with so much at stake.
This article has been updated to take in recent developments
This article is free to read
To unlock more articles, subscribe to get 3 months of unlimited access for just $5







Comments
Join the debate for just £1 a month
Be part of the conversation with other Spectator readers by getting your first three months for £3.
UNLOCK ACCESS Just £1 a monthAlready a subscriber? Log in